CAR T-Cell Therapy in Hematological Cancers: Current Challenges and Future Potential
Although chimeric antigen receptor (CAR) T-cell treatments have shown efficacy in certain cancers, targeting multiple antigens and overcoming production limitations may advance the field and make this therapy more effective and accessible.
Chimeric antigen receptor (CAR) T-cell therapy has been shown effective in hematological cancers, including B-cell leukemia and lymphoma, but relapse is a common occurrence in patients following initial treatment. A review published in Cancer Immunology, Immunotherapy reviewed advanced modifications of basic CAR T-cell therapy and preclinical approaches that hold potential to produce longer-term results.
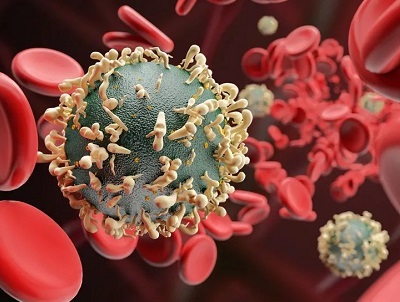
CAR T-cell therapy involves genetically engineering T cells extracted from a patient’s blood to target specific antigens. The cells are then reintroduced via infusion to attack cancer cells. There are currently 3 generations of CAR T-cell therapies, with second- and third-generation options incorporating a primary activation domain plus 1 or 2 costimulatory domains to drive increased T-cell and cytokine production in target cells. Several CAR T-cell therapies targeting the pan B-cell marker CD19, which has significant potential in hematological cancers, are currently approved.
Although CAR T-cell therapy has provided patients with seemingly incurable cancers an option that may be more effective than traditional treatments, high production costs are a limiting factor in widespread adoption of this modality; CAR T-cell drugs run in the hundreds of thousands of dollars for a single infusion. In addition, many patients see relapses that often produce antigen-negative tumors.
There are certain established features in CAR T-cell therapy design that are key to its efficacy, according to the study authors. Choosing an antigen to target is one crucial aspect affecting treatment effectiveness. An antigen that is highly expressed on all tumor cells and that is critical for the survival of malignant cells should be chosen to increase the likelihood of durable treatment response.
Different hematological cancers have seen results with different antigen targets. In acute lymphoblastic leukemia, CD19 is currently considered the most important marker, and high response rates led to the approval of the first CD19-targeting CAR T-cell therapy, tisagenlecleucel (Kymriah). Other currently approved therapies include idecabtagene vicleucel (Abecma), lisocabtagene maraleucel (Breyanzi), brexucabtagene autoleucel (Tecartus), and axicabtagene ciloleucel (Yescarta).
Identifying new potential antigen targets is an important aspect of current and future research.
Patients with chronic lymphocytic leukemia have seen less robust results with CD19 CAR T cells, potentially due to lower initial T-cell function in patients and therefore less efficacy after manufacturing. Combination therapy with ibrutinib is one approach that has been shown to increase response rates in ongoing clinical trials, and other targets are under investigation. B-cell lymphoma is another cancer type that has seen less robust results with CD19 CAR T cells, with ongoing research aiming to identify new targets and increase response.
B-cell maturation antigen (BCMA) is the most researched approach in multiple myeloma, with several trials showing good response rates; however, BCMA-negative tumor relapse has been seen in some studies. Evaluation is currently underway for BCMA CAR T-cells that aim to address this issue. As in other cancer types, additional targets are being explored.
The current CAR T-cell treatment landscape is also limited to therapies targeting a single antigen for hematological cancers, the study authors note. Several options targeting multiple antigens, which may help mitigate relapse by antigen-negative tumors, are in the pipeline and may be the future of CAR T-cell therapy if found safe and effective.
The costimulatory domain selection is also crucial, and most CARs currently being developed use CD28 or 4-1BB costimulatory domains. Cells with a CD28 costimulatory domain have shown quick response and persisted for 3 months in vivo. Those with 4-1BB as a costimulatory domain work more slowly in comparison but have been shown to persist for more than 5 years. Depending on the cancer type and speed of cell proliferation, each of these options could be promising.
Cell quality over quantity has been shown to be key in recent research, with one report seeing a complete patient response due to clonal expansion of a single CD19-directed CAR T cell. T cells with a memory-related gene signature (central memory or stem cell memory phenotypes) have shown more potential to proliferate and survive in patients after infusion.
Calculating optimal dosage is another difficult but important facet of CAR T-cell therapy effectiveness. Because the cells proliferate once infused, determining a linear relationship between dosing and efficacy is complex. Mathematical models have been created to predict minimum effective dosage, but clinical trials are needed to determine their accuracy.
Manufacturing is another area requiring further honing to make CAR T-cell therapy more accessible. As more therapies are approved and demand increases, the current autologous manufacturing process may have to give way to allogeneic cell production to keep up. However, allogeneic production has shown significant risk of graft-versus-host disease that further research must address to ensure the treatment is safe and effective. Allogeneic development also has the potential to reduce costs.
Despite the current drawbacks, the study authors conclude that CAR T-cell therapy has proved to be an important new option for patients with cancer. As issues surrounding relapse and production are addressed, these drugs have potential to push the field forward and produce favorable outcomes.
Reference
Ormhøj M, Abken H, Hadrup SR. Engineering T-cells with chimeric antigen receptors to combat hematological cancers: an update on clinical. Cancer Immunol Immunother. Published online February 23, 2022. doi:10.1007/s00262-022-03163-y
https://www.ajmc.com/view/car-t-cell-therapy-in-hematological-cancers-current-challenges-and-future-potential
Disclaimer:《CAR T-Cell Therapy in Hematological Cancers: Current Challenges and Future Potential》Edited and sorted by Seagull Pharmacy's editors. Please contact us in time if there is any infringement. In addition, the suggestions for drug usage, dosage and disease mentioned in the article are only for medical staff's reference, and can not be used as any basis for medication!